Ocular Migraine Triggers: Common Factors and Practical Ways to Reduce Risk
Introduction
Ocular migraine can feel like the world briefly swapped to a channel of shimmering static. While the visuals can be unsettling, the episode is often short-lived and not a direct sign of eye damage. Understanding what sets these events in motion is a meaningful step toward reducing how often they happen, shortening their duration, or making them less intense. This article explores common triggers and offers realistic, everyday strategies you can tailor to your routine.
Outline
– What ocular migraine is, how it differs from other visual episodes, and why triggers matter
– Light, screens, and visual environments that can nudge the brain toward an aura
– Body rhythms and lifestyle factors, from sleep and stress to hydration and hormones
– Food and chemical exposures: what evidence supports and what remains anecdotal
– A practical prevention plan, including tracking patterns and when to seek care
What Is an Ocular Migraine? Mechanisms, Myths, and Why Triggers Matter
Many people use “ocular migraine” to describe the shimmering patterns, zigzag lines, blind spots, or kaleidoscopic edges that drift across vision and fade within 5–60 minutes. Clinically, these experiences often align with migraine aura, which can appear with or without a headache. A rarer condition called retinal migraine produces transient, usually monocular vision loss or scintillations in one eye; this requires careful medical evaluation, especially if symptoms are prolonged or associated with other neurological changes. For most, however, the classic visual aura reflects brain activity rather than an eye disease: waves of electrical and blood-flow change, called cortical spreading depression, move across the visual cortex at a measured pace (often a few millimeters per minute), matching the marching progress of the visuals people describe.
Why do triggers matter? Migraine is thought to arise from a sensitive brain that responds more strongly to changes in internal and external cues—light shifts, sleep disruption, dehydration, stress swings, hormonal cycles, and certain chemicals. Globally, migraine affects a sizable share of adults, and roughly one in four people with migraine report aura at some point. Triggers do not “cause” migraine in the way a switch flips a lamp; rather, they stack and lower the threshold at which an episode begins. One person might tolerate bright sunlight if well rested and hydrated, yet struggle after a short night and skipped lunch. Because thresholds vary, prevention works best when personalized to your patterns.
Common misconceptions can make management harder than it needs to be:
– “It’s an eye problem only.” In many cases the origin is neurological, even if the visuals feel eye-based.
– “If I avoid one food, I’ll never get another aura.” For most, triggers are multifactorial and context-dependent.
– “All aura means stroke.” Aura is a known migraine feature; however, new, sudden, or severe neurological symptoms—especially weakness, trouble speaking, or a persistent, one-eye blackout—warrant urgent medical assessment.
– “Nothing helps.” While there’s no one-size-fits-all fix, measured adjustments to light exposure, sleep, hydration, meals, and stress often reduce frequency or severity.
Framed this way, identifying triggers is less about restriction and more about fine-tuning the daily environment so your brain encounters fewer jolts and more gentle transitions.
Light, Screens, and Visual Environments: How Brightness and Flicker Spark Symptoms
Light is a frequent nudge for visual aura, especially when it is bright, high-contrast, or rapidly changing. Think of stepping from a dim hallway into midday sun reflecting off water or snow, or the stark contrast of black text on a glowing screen in a dark room. The brain’s visual pathways are sensitive to abrupt shifts in luminance and pattern; for some, that sensitivity can invite an episode. Certain indoor sources can also be provocative: overhead lighting that flickers subtly, blue-rich LEDs at night, or a monitor set too bright for the room. Even when flicker is too fast to notice consciously, the visual system may still register it as stress.
Fortunately, light can be shaped. Outdoors, polarized lenses reduce glare bouncing off horizontal surfaces like water or asphalt. A brimmed hat softens top-down brightness, and seeking shade during peak sun cuts intensity without staying indoors. Inside, balanced lighting (not too dim, not overly bright) reduces contrast against screens. Adjusting position reduces glare from windows; a slight screen tilt can eliminate a reflective hotspot. Many people find comfort with warmer color temperatures in the evening, which can ease visual strain for some, though responses vary.
Screen habits matter as much as settings. Prolonged near work narrows blink rate and can dry the surface of the eyes, increasing discomfort that mimics or compounds trigger load. Regular breaks help the visual system reset.
– Try the “20-20-20” rhythm: every 20 minutes, look at something about 20 feet away for 20 seconds.
– Set screen brightness to match ambient light; avoid extreme contrast.
– Increase text size to reduce squinting and avoid leaning forward.
– Explore high-contrast themes judiciously; too much contrast in a dark room can be fatiguing.
– Position screens perpendicular to windows to minimize glare; use curtains to diffuse midday sun.
Nighttime driving can be challenging due to headlight glare, rain-slick roads, and high contrast. Planning routes that avoid prolonged exposure to bright oncoming lights, keeping windshields clean (inside and out), and moderating speed in wet conditions can reduce the intensity of reflective sparkle. Think of these adjustments not as limitations but as dialing the light to a friendlier setting for a sensitive visual system.
Body Rhythms, Stress, and Physiology: Lifestyle Triggers You Can Tame
Daily rhythms are the quiet architects of migraine vulnerability. Irregular sleep is a well-known contributor: late nights, early wake-ups, or “catch-up” sleep on weekends can all shift the brain’s equilibrium. Even the stress cycle plays a role; many people notice attacks not during peak stress but in the “letdown” afterward, when tension finally unwinds. Skipping meals or long gaps between eating can nudge the body into low glucose states, and dehydration concentrates this effect. For some, hormonal changes—particularly around menstruation—add weight to the trigger stack, which is why timing patterns in a diary can be revealing.
Practical adjustments don’t have to be rigid. Regular sleep and wake times smooth the nervous system’s expectations. A consistent pre-sleep routine helps anchor the clock: dimmer lights, a quiet wind-down, and fewer late-evening screen jolts. Hydration can be folded into existing habits (a glass of water with each meal and after exercise), and keeping snacks with protein and complex carbohydrates handy reduces long fasting intervals. Moderate, regular physical activity is often helpful; it supports sleep quality, mood regulation, and cardiovascular health, all of which can raise the migraine threshold. If exercise itself seems to trigger symptoms, start with shorter durations at lower intensity, warm up thoroughly, and build gradually.
Stress management is less about eliminating pressure and more about improving the body’s recovery from it. Brief, repeatable practices tend to stick:
– Two to five minutes of slow breathing: inhale through the nose for about four counts, exhale for six.
– Short movement breaks: shoulder rolls, gentle neck stretches, or a quick walk to shake out tension.
– Micro-pauses between tasks: look away from the screen, soften the jaw, unclench the hands.
Weather and altitude can also shift the dial. Rapid barometric changes may correspond with attacks in some individuals, and high altitudes or very hot environments add physiologic stress. When you anticipate these conditions, lean on proactive steps—extra fluids, regular small meals, and earlier bedtimes—to blunt the impact. Overall, the goal is steady inputs: predictable sleep, steady nourishment, adequate hydration, and stress-rest cycles that keep your nervous system from swinging between extremes.
Food and Chemical Exposures: Sorting Evidence from Anecdote
Food-related triggers are a frequent topic, but the research picture is nuanced. Some compounds are suspected to lower the migraine threshold in susceptible people—tyramine in aged or fermented items, nitrites in certain processed meats, histamine in wines or long-stored foods, and glutamate found naturally in many ingredients. Alcohol, particularly red varieties, can combine vasodilation with dehydrating effects and sleep disruption. Caffeine is a double-edged tool: small to moderate amounts may help some individuals, while too much—or abrupt withdrawal—can backfire.
The challenge is that dietary effects are highly individual and tangled with context. A glass of wine at the end of a stressful, sleep-deprived day may be more provocative than the same drink on a relaxed evening after a good meal. Similarly, a specific cheese may seem guilty when the real culprit is a skipped lunch or bright afternoon glare that “stacked” with dinner. Rather than banning entire food groups, many people make progress by observing patterns and gently experimenting with timing, portion size, and combinations.
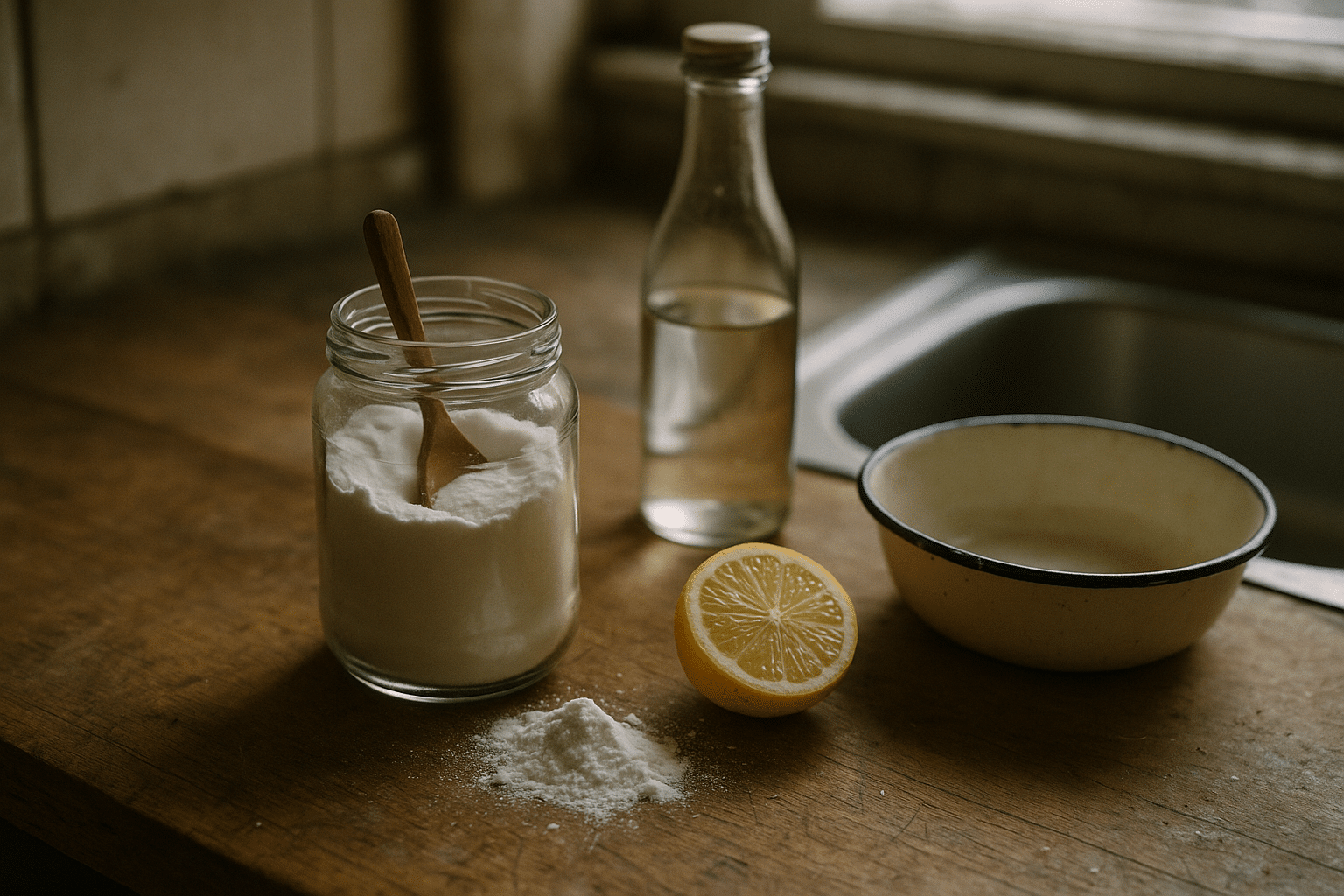
Consider a measured approach:
– Keep a brief diary for 4–6 weeks. Note foods, drinks, timing, sleep, stress, light exposure, and any aura events.
– Look for clusters: Was the episode after prolonged fasting, bright sun, and an aged or fermented food?
– Test changes one at a time: adjust portion size or timing rather than eliminating multiple items at once.
– Build safeguards: drink water with alcohol, pair higher-risk items with a balanced meal, and avoid trying new foods when other triggers are high.
Be cautious of sweeping claims. While some people report clear sensitivities to additives like monosodium glutamate or sweeteners, others find no effect. Evidence supports that consistency—regular meals, steady hydration, and avoiding large swings in caffeine intake—is more reliable than any single “never eat” rule. If you suspect a strong, consistent reaction to a particular item, a structured elimination and reintroduction under guidance can help confirm it. The goal is confidence in your choices, not a shrinking menu.
Your Practical Prevention Plan: Tracking, Thresholds, and Real-World Strategies
Reducing ocular migraine risk works best when you treat triggers as additive. A demanding week plus short sleep, dehydrating coffee-only mornings, and a sunny commute can lower your threshold more than any one factor alone. A simple tracking plan turns guesswork into patterns you can act on. Use a notebook or a phone note—nothing fancy. Write down episode times, last night’s sleep, meals and hydration, stress level, light exposure, and menstrual cycle phase if relevant. After a few weeks, trends emerge that guide choices.
From patterns to actions:
– Stabilize anchors: regular sleep and wake times, scheduled meals or snacks, and a basic hydration target across the day.
– Tame light swings: bring polarized sunglasses, add a hat, and adjust indoor lighting to reduce glare and high contrast.
– Pace screen time: adopt the 20-20-20 habit, increase text size, and match display brightness to the room.
– Preempt travel and weather shifts: pack a water bottle, snacks, and a cap; plan short breaks during long drives.
– Build micro-rests: brief breathing, stretch, or walk breaks between tasks to lower accumulated tension.
If an aura begins, many people find relief by stepping away from bright light, closing the eyes or covering them gently, hydrating, and giving the episode time to pass. A cool compress and a calm, dim space can ease associated discomfort. Because visual aura can overlap with other conditions, seek prompt evaluation for any new or atypical symptoms, especially if vision loss is only in one eye and lasts longer than usual, or if it pairs with weakness, difficulty speaking, or severe sudden headache. Ongoing patterns that disrupt life are worth discussing with a clinician; options may include non-drug strategies, acute treatments for associated headaches, and preventive approaches when attacks are frequent.
Think of this plan as a living document. Your threshold will vary, and that’s expected. By stacking small, sustainable habits—gentler light, steadier sleep, regular fueling, and moments of decompression—you create a buffer between daily life and your visual system. The payoff is fewer surprises, faster recovery, and greater confidence navigating the bright, busy world.